Diabetes is a chronic health condition that affects how your body turns food into energy. When left unmanaged, it can lead to serious health complications such as heart disease, kidney failure, and nerve damage. With millions of people worldwide living with diabetes, understanding its basics is more important than ever.
Table of Contents
In this comprehensive guide, we will explore everything you need to know about diabetes. From its different types and common symptoms to effective diagnosis methods and management strategies, this article aims to empower you with the knowledge needed to take control of your health. Whether you have been recently diagnosed, have a loved one with diabetes, or are simply looking to learn more about this condition, this guide will provide clear and practical information to help you navigate diabetes with confidence.
What Is Diabetes? A Comprehensive Overview
Types of Diabetes
Diabetes is not a one-size-fits-all condition; it encompasses several distinct types, each with unique causes, characteristics, and management approaches. Understanding these types is crucial for effective prevention and treatment.
Type 1 Diabetes
Description: Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This results in little to no insulin being produced, and individuals with Type 1 diabetes must rely on insulin injections or an insulin pump for the rest of their lives.
Causes: The exact cause is not known, but it is believed to involve a combination of genetic predisposition and environmental factors, such as viruses, which trigger the autoimmune response.
Symptoms: Common symptoms include excessive thirst, frequent urination, weight loss, fatigue, blurred vision, and irritability. Symptoms can appear suddenly and may worsen quickly.
Treatment and Management: People with Type 1 diabetes need lifelong insulin therapy. They also need to closely monitor their blood glucose levels, adjust insulin doses based on food intake and activity, and adopt a balanced diet and exercise plan.
Type 2 Diabetes
Description: Type 2 diabetes is the most common form, accounting for around 90-95% of all diabetes cases. It occurs when the body becomes resistant to insulin or when the pancreas can no longer produce enough insulin to maintain normal blood sugar levels.
Causes: Type 2 diabetes is strongly associated with lifestyle factors such as obesity, physical inactivity, poor diet, and genetics. However, aging, family history, and ethnicity (e.g., African American, Hispanic, or Native American) can increase the risk.
Symptoms: Symptoms often develop slowly and can include increased thirst, frequent urination, slow-healing wounds, fatigue, and numbness or tingling in the hands or feet. Sometimes, individuals may not experience noticeable symptoms until the condition is advanced.
Treatment and Management: While Type 2 diabetes can often be managed with lifestyle changes, such as regular exercise and a healthy diet, some individuals may need oral medications or insulin to regulate blood sugar levels. Blood glucose monitoring is essential for managing the condition effectively.
Gestational Diabetes
Description: Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased needs during this time. It affects around 2-10% of pregnancies and usually goes away after childbirth. However, it increases the risk of developing Type 2 diabetes later in life for both the mother and the child.
Causes: The exact cause is unclear, but hormonal changes during pregnancy play a role in insulin resistance. Genetics and lifestyle factors also contribute to the risk.
Symptoms: Gestational diabetes often has no symptoms, which is why screening during pregnancy is vital. If symptoms occur, they may include excessive thirst, frequent urination, and fatigue.
Treatment and Management: Managing gestational diabetes involves maintaining a healthy diet, engaging in regular physical activity, and monitoring blood sugar levels. In some cases, insulin or oral medications may be required. After delivery, blood sugar levels typically return to normal, but regular follow-up is recommended to monitor the development of Type 2 diabetes.
Prediabetes
Description: Prediabetes is a condition where blood sugar levels are higher than normal but not yet high enough to be classified as Type 2 diabetes. It is often a precursor to Type 2 diabetes and signals an increased risk of developing the full-blown disease in the future.
Causes: Prediabetes shares many of the same risk factors as Type 2 diabetes, such as being overweight, having a sedentary lifestyle, or a family history of diabetes.
Symptoms: There are typically no symptoms of prediabetes, which is why regular screening is important. Without intervention, it can progress to Type 2 diabetes.
Treatment and Management: The good news is that prediabetes is reversible. By adopting a healthy diet, increasing physical activity, losing weight, and making other lifestyle changes, individuals can significantly lower their risk of progressing to Type 2 diabetes.
LADA (Latent Autoimmune Diabetes in Adults)
Description: Often considered a hybrid form of Type 1 and Type 2 diabetes, LADA is a slow-progressing form of autoimmune diabetes that typically develops in adulthood. It shares characteristics with both Type 1 and Type 2, as individuals with LADA have insulin resistance and an autoimmune response that affects the pancreas.
Causes: The causes of LADA are not fully understood, but it is believed to involve a combination of genetic and environmental factors, similar to Type 1 diabetes, with some degree of insulin resistance, like Type 2 diabetes.
Symptoms: LADA symptoms can initially resemble Type 2 diabetes, such as increased thirst and frequent urination, but it progresses more rapidly, and insulin therapy may eventually be required.
Treatment and Management: LADA is treated with insulin therapy, and people with LADA also need to manage blood sugar levels through diet and lifestyle changes. Monitoring is crucial, as insulin dependence can develop more quickly compared to Type 2 diabetes.
Maturity-Onset Diabetes of the Young (MODY)
Description: MODY is a rare form of diabetes that is typically diagnosed in adolescence or early adulthood and is caused by a genetic mutation. Unlike Type 1 and Type 2, MODY is not related to insulin resistance or autoimmune processes.
Causes: MODY is caused by a mutation in a single gene, which results in the pancreas producing insufficient insulin. It is inherited in an autosomal dominant pattern, meaning that a child has a 50% chance of inheriting the condition if one parent has it.
Symptoms: MODY symptoms can be similar to those of Type 1 or Type 2 diabetes but tend to be less severe. Individuals with MODY may be able to manage their condition with lifestyle changes or oral medications rather than insulin.
Treatment and Management: Treatment varies depending on the specific genetic mutation but can often involve lifestyle modifications and oral medications to help regulate blood sugar levels.
The Role of Insulin in Diabetes
What is Insulin?
Insulin is a peptide hormone produced by beta cells in the pancreas, located behind the stomach. After food is consumed, especially foods rich in carbohydrates, the body breaks down these nutrients into glucose, which enters the bloodstream. In response, the pancreas releases insulin into the bloodstream, where it helps glucose move from the blood into cells throughout the body, particularly muscle, liver, and fat cells. These cells then either use glucose for energy or store it for future use.
Insulin’s Role in the Body
– Regulation of Blood Sugar: Insulin helps maintain stable blood sugar levels by facilitating the entry of glucose into cells. Without insulin, the body’s cells cannot absorb glucose, leading to elevated blood sugar levels.
– Energy Production and Storage: Once inside the cells, glucose is either used immediately for energy or stored in the liver and muscles as glycogen for later use. Insulin ensures that excess glucose is stored efficiently, preventing a rise in blood sugar.
– Fat and Protein Metabolism: Besides controlling glucose, insulin also influences fat and protein metabolism. It promotes the storage of fat in adipose tissue and helps the body use proteins to repair tissues and build muscles.
The Disruption of Insulin Function in Diabetes
In people with diabetes, there are two main scenarios in which insulin function is compromised:
– In Type 1 Diabetes: The body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas, leading to little or no insulin production. This forces individuals to rely on insulin injections or pumps for blood sugar regulation.
– In Type 2 Diabetes: The body becomes resistant to insulin, meaning the cells no longer respond to the hormone as effectively. The pancreas tries to compensate by producing more insulin, but over time, it may not produce enough to keep blood sugar levels within a normal range.
Consequences of Insulin Imbalance
– High Blood Sugar (Hyperglycemia): When insulin is not effectively used or produced, glucose accumulates in the blood, leading to hyperglycemia. Over time, high blood sugar can damage vital organs, including the heart, kidneys, nerves, and eyes.
– Low Blood Sugar (Hypoglycemia): On the other hand, an excess of insulin or insulin therapy can cause blood sugar levels to drop too low, resulting in hypoglycemia. Symptoms of hypoglycemia include shaking, sweating, confusion, and in severe cases, loss of consciousness or seizures.
Insulin Therapy in Diabetes Management
– Type 1 Diabetes: People with Type 1 diabetes must take insulin every day through injections or an insulin pump. This external insulin helps regulate their blood sugar, as their pancreas no longer produces the hormone.
– Type 2 Diabetes: In the early stages, lifestyle changes such as diet and exercise may improve insulin sensitivity. However, some individuals with Type 2 diabetes may eventually require insulin injections or other medications that help the body use insulin more effectively.
Insulin Sensitivity and Resistance
– Insulin Sensitivity: A person with good insulin sensitivity requires less insulin to regulate blood sugar. Regular physical activity, a balanced diet, and maintaining a healthy weight can improve insulin sensitivity.
– Insulin Resistance: In Type 2 diabetes, the body’s cells become less responsive to insulin, leading to insulin resistance. To overcome this, the pancreas produces more insulin, but eventually, it cannot keep up with the demand, leading to elevated blood sugar levels.
The Future of Insulin and Diabetes Care
Researchers are continuously working on new ways to improve insulin therapy and diabetes management. Innovations like artificial pancreas systems, which combine insulin pumps with continuous glucose monitors, and potential oral insulin, are helping improve the lives of those with diabetes.
Additionally, promising treatments that focus on improving insulin sensitivity and targeting insulin resistance through medications or lifestyle changes are enhancing the quality of life for individuals with Type 2 diabetes.
How Diabetes Affects the Body
Impact on the Pancreas
The pancreas is central to blood sugar regulation as it produces insulin, a hormone that helps cells absorb glucose from the bloodstream. In diabetes, the function of the pancreas is severely impacted:
– In Type 1 Diabetes: The body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. As a result, people with Type 1 diabetes either produce very little or no insulin at all. Insulin is necessary for regulating blood sugar, so individuals with Type 1 diabetes must rely on insulin injections or pumps for life.
– In Type 2 Diabetes: In the early stages, the pancreas compensates by producing more insulin to overcome insulin resistance in the body’s cells. Over time, however, the pancreas may become overworked and unable to produce enough insulin to manage blood sugar levels effectively. This leads to high blood sugar, which is characteristic of Type 2 diabetes.
If the pancreas becomes damaged over time due to chronic high blood sugar levels, insulin production can be further impaired, making diabetes more difficult to manage and increasing the risk of complications.
Impact on Blood Sugar Levels
Insulin is the key hormone responsible for moving glucose from the blood into cells, where it is used for energy. In diabetes, this process is disrupted:
– In Type 1 Diabetes: With insufficient or absent insulin production, glucose remains in the bloodstream instead of being absorbed by the cells. This results in elevated blood sugar levels (hyperglycemia).
– In Type 2 Diabetes: The body’s cells become resistant to insulin, and the pancreas struggles to keep up with the demand for insulin production. As a result, blood sugar levels rise. Over time, the body’s ability to regulate blood sugar becomes increasingly ineffective.
Uncontrolled blood sugar levels can lead to a variety of short-term and long-term health issues. Chronically elevated blood sugar can damage blood vessels and organs, while episodes of very low blood sugar (hypoglycemia) can cause symptoms like confusion, dizziness, and, in severe cases, loss of consciousness.
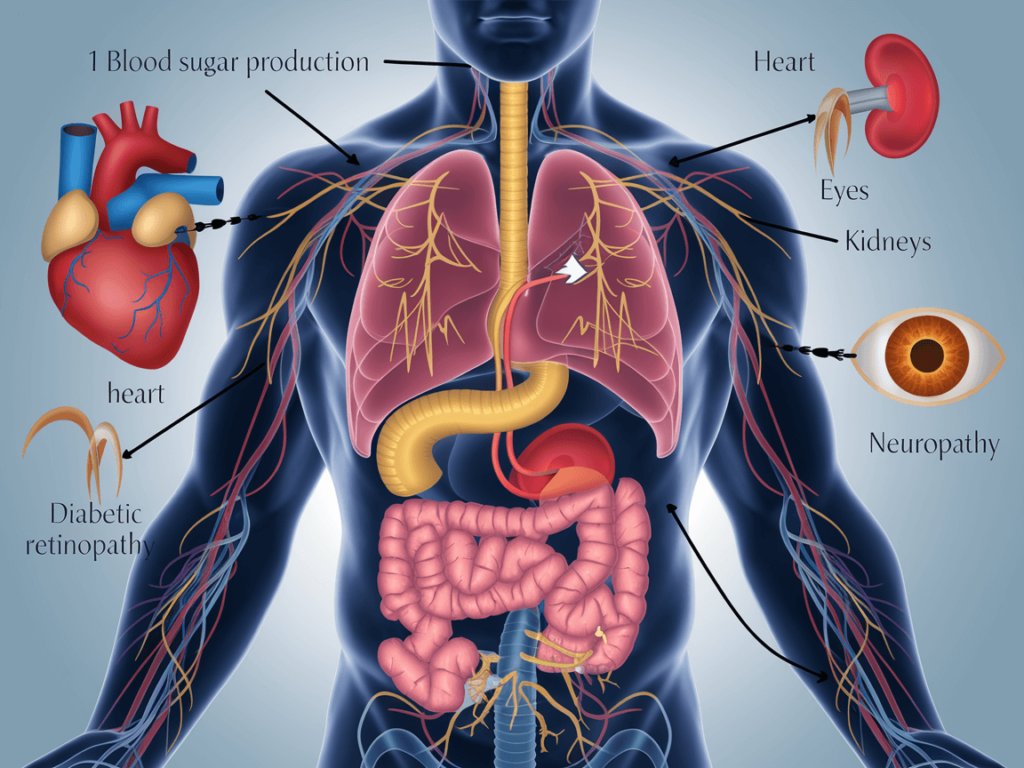
Impact on Organs and Systems
Diabetes affects nearly every organ system in the body. The long-term consequences of poorly controlled blood sugar can lead to serious complications:
– Heart and Blood Vessels: High blood sugar can damage the lining of blood vessels, increasing the risk of heart disease and stroke. People with diabetes are more likely to develop high blood pressure, which further elevates the risk of cardiovascular complications.
– Kidneys: Over time, high blood sugar can damage the kidneys’ filtering system, leading to diabetic nephropathy. This can progress to kidney failure if not managed effectively, requiring dialysis or a kidney transplant.
– Eyes: Diabetes can damage the blood vessels in the retina, leading to diabetic retinopathy, which can cause blindness if left untreated. High blood sugar levels can also increase the risk of cataracts and glaucoma.
– Nerves: Chronic high blood sugar can cause damage to the nerves, a condition known as diabetic neuropathy. This can lead to symptoms such as numbness, tingling, pain, and weakness, particularly in the hands and feet. In severe cases, diabetic neuropathy can lead to amputation due to infections in the feet.
– Feet and Skin: Nerve damage can reduce sensation in the feet, making it harder for people with diabetes to detect injuries or infections. Poor circulation due to high blood sugar can also slow healing, leading to complications like ulcers, infections, and, in severe cases, amputations.
Brief Mention of Complications
– Diabetic Retinopathy: High blood sugar can cause damage to the blood vessels in the retina, leading to diabetic retinopathy. Early stages may not show symptoms, but as the condition progresses, it can cause vision problems, including blindness. Regular eye exams are essential for early detection and treatment.
– Diabetic Neuropathy: Prolonged high blood sugar levels can damage the nerves, especially in the hands and feet. Symptoms may include pain, tingling, numbness, and loss of sensation. If left untreated, neuropathy can lead to severe complications, such as foot ulcers, infections, and amputations.
Understanding Diabetes Symptoms and Early Signs
Common Symptoms of Diabetes
– Increased Thirst (Polydipsia)
One of the earliest symptoms of diabetes is excessive thirst, medically known as polydipsia. When blood sugar levels are consistently high, the kidneys work overtime to filter and remove excess glucose from the bloodstream. This process increases urine production, leading to dehydration. To compensate for this fluid loss, the body signals the need for more water, which results in increased thirst.
Why it happens: When the kidneys filter excess glucose, they draw water from the bloodstream to flush it out through urine, leaving the body dehydrated.
What to look for: If you find yourself constantly thirsty and unable to quench your thirst, this could be a sign that your blood sugar is elevated.
– Frequent Urination (Polyuria)
Increased urination, known as polyuria, is closely related to increased thirst. As the kidneys attempt to filter excess glucose from the bloodstream, they produce more urine. This frequent urination can lead to further dehydration, which then triggers more thirst.
Why it happens: The kidneys filter glucose into urine, drawing additional water with it, which increases urine volume.
What to look for: Frequent visits to the bathroom, particularly during the night (nocturia), can be a red flag for diabetes.
– Fatigue
Fatigue is a common and often overlooked symptom of diabetes. People with high blood sugar may feel unusually tired or lethargic because their bodies are not able to use glucose effectively for energy. Glucose is the body’s primary energy source, but when insulin resistance or insufficient insulin production occurs, the cells cannot absorb glucose properly.
Why it happens: When glucose cannot enter the cells due to insulin problems, the body’s energy production is reduced, leading to fatigue.
What to look for: Persistent tiredness or feeling drained, even after a full night’s sleep, can be a sign of uncontrolled diabetes.
– Unexplained Weight Loss
Despite eating normally or even more than usual, people with uncontrolled diabetes may experience unexplained weight loss. This occurs because the body begins to break down muscle and fat for energy since it is not able to use glucose effectively due to a lack of insulin or insulin resistance.
Why it happens: Without enough insulin, the body starts using fat and muscle tissue for fuel. The kidneys also excrete excess glucose, which can lead to a loss of calories.
What to look for: Significant weight loss without changes in diet or exercise habits should be considered a warning sign, particularly if it occurs alongside other symptoms like thirst and frequent urination.
– Blurred Vision
Blurred vision is another symptom that may signal the onset of diabetes. High blood sugar levels can cause fluid to be pulled from the lenses of the eyes, affecting the ability to focus. This can lead to temporary blurred vision, which might improve when blood sugar levels are stabilized.
Why it happens: High blood sugar levels draw fluid away from various tissues, including the eyes. This disrupts the ability of the eyes to focus, leading to blurred vision.
What to look for: If you experience sudden or gradual changes in vision, such as blurriness or difficulty focusing, it could be related to elevated blood sugar levels.
How to Recognize Early Warning Signs
– Importance of Monitoring for Early Detection
Monitoring blood sugar levels regularly is critical for the early detection of diabetes, especially since many individuals with early-stage diabetes or pre-diabetes do not exhibit obvious symptoms. Early detection allows for prompt intervention, which can prevent the disease from progressing and reduce the risk of serious complications like heart disease, kidney failure, nerve damage, and vision loss. Regular screening can identify abnormal blood sugar levels before they cause significant harm, allowing for lifestyle changes or medication to help manage the condition effectively. By catching diabetes early, individuals have a much better chance of controlling their blood sugar levels and maintaining a good quality of life.
When to Seek Medical Help
–Knowing When Symptoms Require Professional Evaluation:
Recognizing when symptoms warrant a visit to a healthcare provider is essential for early diagnosis and treatment of diabetes. While many of the common symptoms, such as increased thirst, frequent urination, and fatigue, can initially be mild or mistaken for other conditions, they should not be ignored. If any of these symptoms persist or worsen over time, it’s important to seek medical help.
Uncontrolled or severe symptoms: If symptoms like thirst, fatigue, or blurred vision become increasingly bothersome or don’t improve with hydration or rest, it’s important to seek a professional evaluation.
Unexpected weight loss or extreme hunger: Unexplained weight loss or increased hunger can be signs of undiagnosed diabetes and should be evaluated.
Symptoms affecting daily life: If symptoms interfere with daily activities or quality of life, such as difficulty seeing clearly or persistent numbness in the extremities, it’s time to consult a healthcare provider for testing.
Early medical evaluation can lead to timely diagnosis, appropriate treatment, and prevention of serious complications. Don’t wait for symptoms to become severe—catching them early can make a significant difference in long-term health outcomes.
Diabetes Diagnosis: How It Is Identified
1- Blood Glucose Tests
Fasting Blood Glucose (FBG) and Random Glucose Test
Blood glucose tests are essential tools for diagnosing and managing diabetes. Two of the most commonly used tests are the Fasting Blood Glucose (FBG) test and the Random Blood Glucose (RBG) test. These tests measure the concentration of glucose (sugar) in the blood and help detect abnormal blood sugar levels that may indicate diabetes or prediabetes.
Fasting Blood Glucose (FBG) Test:
The FBG test measures blood sugar levels after an individual has not eaten or consumed any caloric drinks for at least 8 hours. It is typically conducted in the morning before breakfast.
- Purpose: This test helps determine how well the body regulates blood sugar without the influence of recent food intake.
- Procedure: A small blood sample is taken, usually from a vein in the arm, and analyzed for glucose concentration.
- Normal Range:
- Normal: Less than 100 mg/dL (5.6 mmol/L)
- Prediabetes: 100–125 mg/dL (5.6–6.9 mmol/L)
- Diabetes: 126 mg/dL (7.0 mmol/L) or higher on two separate tests
Significance: Elevated fasting blood glucose levels indicate that the body may not be producing enough insulin or is not using insulin efficiently, which are key markers of diabetes.
Random Blood Glucose (RBG) Test:
The Random Blood Glucose test measures blood sugar levels at any time of the day, regardless of when the person last ate. This makes it a convenient and quick method for assessing blood glucose levels.
- Purpose: It helps detect significantly high blood sugar levels, especially when a person is experiencing symptoms of diabetes like excessive thirst, frequent urination, or unexplained fatigue.
- Procedure: A blood sample is taken at any random time without fasting.
- Diagnostic Levels:
- Normal: Typically less than 140 mg/dL (7.8 mmol/L)
- Diabetes: 200 mg/dL (11.1 mmol/L) or higher, especially if accompanied by symptoms of high blood sugar
Significance: A very high random blood sugar level, especially with symptoms of hyperglycemia, may prompt further testing for diabetes.
2- A1C Test
What Is the HbA1c Test?
The HbA1c test, also known as the A1C test or glycated hemoglobin test, is a simple blood test that measures the average blood glucose (sugar) levels over the past 2 to 3 months. It does this by assessing the percentage of hemoglobin—the protein in red blood cells that carries oxygen—that has glucose attached to it.
- How It Works: When blood sugar levels are high, more glucose binds to hemoglobin. Since red blood cells live for about 3 months, the HbA1c test reflects long-term blood sugar control rather than day-to-day fluctuations.
- Test Procedure: A small blood sample is taken from a vein or through a finger prick. Fasting is not required, making it a convenient option.
- Normal and Diagnostic Ranges:
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher on two separate tests
How the HbA1c Test Helps Diagnose and Manage Diabetes
The HbA1c test is a crucial tool for both diagnosing diabetes and monitoring long-term blood sugar control in people already diagnosed with the condition.
1. Diagnosing Diabetes and Prediabetes
- The A1C test is widely used to diagnose Type 1, Type 2, and prediabetes.
- It provides a clearer picture of blood sugar trends than a single blood glucose reading.
- Since it does not require fasting, it’s more convenient than fasting glucose or glucose tolerance tests.
2. Monitoring Diabetes Management
For individuals living with diabetes, the A1C test is essential for evaluating how well blood sugar is being managed over time.
- Tracking Progress: Regular testing (usually every 3 to 6 months) helps track how well medications, diet, and exercise are controlling blood sugar.
- Adjusting Treatment Plans: If the A1C level remains high, healthcare providers may adjust medications or recommend lifestyle changes.
- Reducing Risk of Complications: Keeping A1C levels within the target range (often below 7% for many adults) significantly lowers the risk of diabetes-related complications, such as nerve damage, kidney disease, and vision problems.
3. Setting Personalized Goals
Healthcare providers often set personalized A1C targets based on factors like age, overall health, and the presence of diabetes complications.
- Younger, healthier individuals may aim for an A1C closer to 6.5%.
- Older adults or those with other health conditions may have a slightly higher target to reduce the risk of low blood sugar (hypoglycemia).
3- Oral Glucose Tolerance Test (OGTT)
How the Test Works
The Oral Glucose Tolerance Test (OGTT) is a diagnostic tool used to assess how well the body processes glucose. It measures the body’s ability to regulate blood sugar after consuming a concentrated glucose solution. This test is particularly effective in identifying diabetes and prediabetes.
Step-by-Step Procedure:
- Fasting: The patient must fast (no food or drink except water) for at least 8 hours before the test.
- Initial Blood Sample: A baseline blood sample is taken to measure fasting blood glucose levels.
- Glucose Consumption: The patient drinks a solution containing 75 grams of glucose (for adults). For pregnant women, the solution may vary.
- Blood Sugar Monitoring: Blood samples are taken at specific intervals—typically after 1 hour and 2 hours—to measure how blood sugar levels rise and fall.
Normal and Diagnostic Ranges:
- Normal: Blood glucose is below 140 mg/dL (7.8 mmol/L) after 2 hours.
- Prediabetes: Blood glucose is between 140–199 mg/dL (7.8–11.0 mmol/L) after 2 hours.
- Diabetes: Blood glucose is 200 mg/dL (11.1 mmol/L) or higher after 2 hours.
When It’s Needed
The OGTT is used when other blood sugar tests (like fasting glucose or A1C) do not provide a clear diagnosis. It helps detect how the body handles glucose over time, making it especially useful for specific situations:
1. Diagnosing Type 2 Diabetes and Prediabetes
- The OGTT can detect impaired glucose tolerance (IGT), an early indicator of prediabetes, before more serious symptoms develop.
- It helps confirm Type 2 diabetes when fasting glucose or A1C results are borderline.
2. Diagnosing Gestational Diabetes
- The OGTT is the standard test for diagnosing gestational diabetes during pregnancy.
- Pregnant women typically undergo this test between 24 and 28 weeks of pregnancy to check how their bodies manage glucose, ensuring the health of both mother and baby.
3. Evaluating Reactive Hypoglycemia
- For patients who experience symptoms of low blood sugar after eating, the OGTT can help diagnose reactive hypoglycemia, a condition where blood sugar drops abnormally after meals.
4. Monitoring Patients with Risk Factors
- Individuals with a family history of diabetes, obesity, or polycystic ovary syndrome (PCOS) may need an OGTT if other tests are inconclusive.
- It’s also used to monitor those with metabolic syndrome or other conditions that increase diabetes risk.
Effective Diabetes Management: Tips for a Healthy Life

Diet and Nutrition for Diabetes
Proper diet and nutrition are fundamental for managing diabetes and maintaining stable blood sugar levels. Making informed food choices helps prevent blood sugar spikes, supports weight management, and reduces the risk of diabetes-related complications. A well-balanced diet can also improve overall health and energy levels.
Foods to Focus On
A diabetes-friendly diet emphasizes nutrient-dense foods that are rich in fiber, vitamins, and minerals while being low in added sugars and unhealthy fats. The following food groups are essential for blood sugar control and overall well-being:
1. Whole Grains
Whole grains are high in fiber, which slows digestion and helps prevent rapid spikes in blood sugar. Unlike refined grains, they retain their bran and germ, providing more nutrients.
- Examples: Brown rice, quinoa, oatmeal, whole wheat bread, barley, and bulgur.Effective Diabetes
- Benefits: Stabilizes blood sugar, supports digestion, and keeps you full longer.
2. Fruits (in Moderation)
Fruits provide essential vitamins, minerals, and fiber, but they should be consumed in moderation due to their natural sugar content.
- Examples: Berries (blueberries, strawberries), apples, pears, oranges, and kiwis.
- Benefits: Rich in antioxidants and fiber, fruits help combat inflammation and support heart health.
3. Non-Starchy Vegetables
Non-starchy vegetables are low in carbohydrates and calories, making them ideal for managing blood sugar.
- Examples: Leafy greens (spinach, kale), broccoli, cauliflower, zucchini, and bell peppers.
- Benefits: Provide fiber, vitamins, and minerals without significantly impacting blood glucose levels.
4. Lean Proteins
Including lean protein in meals helps stabilize blood sugar and promotes satiety.
- Examples: Skinless poultry, fish, tofu, legumes, beans, and eggs.
- Benefits: Supports muscle health and helps balance blood sugar when paired with carbohydrates.
5. Healthy Fats
Unsaturated fats support heart health and improve insulin sensitivity when consumed in moderation.
- Examples: Avocados, nuts, seeds, olive oil, and fatty fish (salmon, mackerel).
- Benefits: Reduce inflammation and lower the risk of cardiovascular disease.
Foods to Avoid
Certain foods can cause blood sugar spikes and increase the risk of diabetes complications. Minimizing or eliminating these foods is essential for effective diabetes management.
1. Processed Sugars
Foods and drinks high in added sugars can cause rapid increases in blood glucose levels.
- Examples: Sugary drinks (sodas, energy drinks), candies, pastries, cakes, and sweetened cereals.
- Risks: Leads to poor blood sugar control, weight gain, and increased risk of insulin resistance.
2. Refined Carbohydrates
Refined carbs are stripped of fiber and nutrients, causing quick digestion and blood sugar spikes.
- Examples: White bread, white rice, pasta made from refined flour, pastries, and snack chips.
- Risks: Rapid blood sugar increases followed by crashes, which can worsen insulin sensitivity.
3. Trans Fats and Saturated Fats
These unhealthy fats raise LDL (bad) cholesterol and increase the risk of heart disease, a common complication of diabetes.
- Examples: Fried foods, baked goods with hydrogenated oils, margarine, and processed snacks.
- Risks: Increases inflammation, insulin resistance, and cardiovascular risk.
4. High-Sodium Foods
Excess salt can raise blood pressure and stress the kidneys, organs already at risk in diabetes.
- Examples: Processed meats (bacon, sausages), canned soups, fast food, and salty snacks.
- Risks: Increases the risk of hypertension and kidney damage.
Physical Activity and Diabetes
Regular physical activity is a vital part of managing diabetes and maintaining overall health. Exercise helps regulate blood sugar levels, improves insulin sensitivity, and lowers the risk of diabetes-related complications. By staying active, individuals with diabetes can enhance their quality of life and reduce the need for medication.
Recommended Exercises to Control Blood Sugar
Incorporating a variety of exercises into a fitness routine can effectively help manage blood glucose levels. The key is to balance aerobic, strength, and flexibility exercises for optimal health benefits.
1. Aerobic Exercises (Cardio)
Aerobic exercises increase heart rate and improve circulation, helping the body use insulin more efficiently.
- Examples: Brisk walking, jogging, cycling, swimming, dancing, and hiking.
- Duration: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week (e.g., 30 minutes a day, 5 days a week).
- Benefits: Lowers blood glucose levels, improves heart health, and aids in weight management.
2. Strength Training (Resistance Exercises)
Building muscle through strength training increases insulin sensitivity and supports better glucose uptake by muscles.
- Examples: Weightlifting, resistance band exercises, bodyweight movements (push-ups, squats), and Pilates.
- Frequency: At least 2–3 times per week, with a focus on all major muscle groups.
- Benefits: Enhances muscle mass, improves metabolism, and supports long-term blood sugar control.
3. Flexibility and Balance Exercises
Flexibility and balance exercises reduce the risk of injury and improve joint health, which is important for people with diabetes.
- Examples: Yoga, stretching routines, tai chi, and balance drills.
- Benefits: Reduces stress, enhances flexibility, and improves balance to prevent falls.
4. Light Physical Activities
In addition to structured exercise, increasing daily movement can help manage blood sugar.
- Examples: Taking the stairs, gardening, walking after meals, and household chores.
- Benefits: Reduces blood sugar spikes after eating and encourages an active lifestyle.
The Importance of Regular Activity in Preventing Complications
Consistent physical activity offers powerful protection against the long-term complications associated with diabetes. By staying active, individuals can significantly lower their risk of developing severe health issues.
1. Improves Insulin Sensitivity
Regular exercise allows the body to use insulin more effectively, reducing insulin resistance, especially in people with Type 2 diabetes. This leads to better blood sugar control and may lower the need for medication.
2. Prevents Cardiovascular Disease
Diabetes increases the risk of heart disease and stroke. Exercise strengthens the heart, lowers blood pressure, reduces bad cholesterol (LDL), and increases good cholesterol (HDL), protecting against cardiovascular complications.
3. Supports Weight Management
Maintaining a healthy weight is crucial for diabetes management. Regular activity helps burn calories, reduce body fat, and build lean muscle, all of which contribute to better glucose regulation.
4. Reduces the Risk of Nerve Damage (Neuropathy)
Improved blood flow from regular exercise helps prevent or slow the progression of nerve damage, a common diabetes complication. This is especially important for foot health and balance.
5. Enhances Mental Health
Physical activity reduces stress, anxiety, and depression, which can negatively impact blood sugar control. Exercise also promotes better sleep and overall mental well-being.
6. Lowers the Risk of Kidney and Eye Complications
By improving blood pressure and blood sugar control, regular exercise can help protect the kidneys and eyes from diabetes-related damage (e.g., diabetic nephropathy and retinopathy).
Medications for Diabetes
Medications are essential in managing diabetes, especially when lifestyle changes alone are not enough to maintain healthy blood sugar levels. The type of medication prescribed depends on the type of diabetes, blood sugar levels, and individual health needs. Treatment options include oral medications for Type 2 diabetes and insulin therapy for both Type 1 and advanced Type 2 diabetes.
Overview of Insulin and Oral Medications Like Metformin
1. Insulin Therapy
Insulin is a hormone that helps regulate blood sugar by allowing glucose to enter the body’s cells for energy. People with Type 1 diabetes require insulin because their bodies do not produce it. Some individuals with Type 2 diabetes may also need insulin when other treatments are not enough.
Types of Insulin:
- Rapid-acting insulin: Works quickly to manage blood sugar spikes during meals. (e.g., insulin lispro, insulin aspart)
- Short-acting insulin: Taken before meals to control post-meal blood sugar. (e.g., regular insulin)
- Intermediate-acting insulin: Covers blood sugar needs for about half a day or overnight. (e.g., NPH insulin)
- Long-acting insulin: Provides steady insulin levels throughout the day and night. (e.g., insulin glargine, insulin detemir)
- Premixed insulin: Combines two types of insulin for convenience.
Delivery Methods:
- Insulin injections using syringes or insulin pens.
- Insulin pumps that deliver continuous doses.
- Inhaled insulin for rapid action during meals.
2. Oral Medications (Focus on Metformin)
Metformin is the most commonly prescribed oral medication for Type 2 diabetes. It works by:
- Reducing glucose production in the liver.
- Improving insulin sensitivity in muscle cells.
- Lowering blood sugar levels without causing weight gain.
Other Common Oral Medications Include:
- Sulfonylureas: Stimulate the pancreas to release more insulin. (e.g., glipizide, glyburide)
- DPP-4 Inhibitors: Help increase insulin production and decrease sugar release. (e.g., sitagliptin, linagliptin)
- SGLT2 Inhibitors: Prevent the kidneys from reabsorbing glucose, leading to sugar excretion through urine. (e.g., canagliflozin, dapagliflozin)
- Thiazolidinediones (TZDs): Improve insulin sensitivity. (e.g., pioglitazone)
These medications are often combined for better blood sugar control, depending on the patient’s condition.
The Role of Insulin Therapy and Blood Sugar Monitoring
1. Insulin Therapy in Diabetes Management
Insulin therapy is vital for individuals whose bodies cannot produce or use insulin effectively. It helps maintain blood sugar within a safe range and prevents serious complications. Proper insulin use:
- Prevents hyperglycemia (high blood sugar) and diabetic ketoacidosis in Type 1 diabetes.
- Reduces the risk of long-term complications like nerve damage, kidney disease, and eye problems.
- Provides flexibility in managing blood sugar, especially with meal planning and physical activity.
2. Importance of Blood Sugar Monitoring
Regular blood sugar monitoring is essential for people using insulin and other diabetes medications. It helps track how treatments and lifestyle choices affect glucose levels.
Monitoring Methods:
- Fingerstick testing with a glucose meter for daily checks.
- Continuous Glucose Monitors (CGMs): Devices that track glucose levels throughout the day in real-time.
- Flash glucose monitors: Allow quick scans to check glucose trends.
Benefits of Monitoring:
- Adjusts medication dosages as needed.
- Detects hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) early.
- Helps manage diet, exercise, and insulin timing effectively.
Preventing Diabetes: What You Can Do to Stay Healthy
Healthy Eating Habits
Developing healthy eating habits is a cornerstone of effective diabetes management. Eating well-balanced meals in appropriate portions helps regulate blood sugar levels, maintain a healthy weight, and reduce the risk of diabetes-related complications. Understanding how to balance nutrients and control portion sizes empowers individuals to make better food choices and maintain stable energy throughout the day.
Balanced Meals
A balanced diet ensures the body receives the right combination of macronutrients (carbohydrates, proteins, and fats) and micronutrients (vitamins and minerals) to support overall health and blood sugar control.
1. Carbohydrates:
Carbohydrates have the most direct impact on blood sugar levels, so choosing the right types and amounts is critical.
- Focus on: Whole grains (quinoa, brown rice, whole wheat bread), legumes (lentils, beans), fruits, and vegetables.
- Limit: Refined carbs (white bread, pastries), sugary drinks, and processed snacks.
- Tip: Pair carbs with protein or healthy fats to slow sugar absorption and prevent spikes in blood glucose.
2. Proteins:
Protein helps with satiety and muscle maintenance without significantly affecting blood sugar.
- Healthy options: Lean meats (chicken, turkey), fish, tofu, eggs, legumes, and low-fat dairy.
- Benefit: Including protein in meals stabilizes blood sugar and prevents overeating.
3. Healthy Fats:
Unsaturated fats improve heart health and can help manage cholesterol levels.
- Healthy fats: Avocados, nuts, seeds, olive oil, and fatty fish like salmon.
- Limit: Saturated and trans fats found in fried foods, butter, and processed snacks.
4. Fiber:
Fiber slows digestion and helps manage blood sugar spikes.
- Sources: Vegetables, fruits with skins, whole grains, legumes, and seeds.
- Benefit: Improves digestion and promotes feelings of fullness.
5. Hydration:
Staying hydrated supports overall health and helps regulate blood sugar.
- Best choices: Water, herbal teas, and infused water with lemon or cucumber.
- Avoid: Sugary drinks and excessive fruit juices.
The Plate Method for Balanced Meals:
An easy way to create balanced meals is to use the Diabetes Plate Method:
- Half the plate: Non-starchy vegetables (spinach, broccoli, peppers).
- One-quarter: Lean protein (chicken, fish, tofu).
- One-quarter: Healthy carbohydrates (quinoa, brown rice, beans).
- Add a small serving of healthy fat (olive oil, avocado).
- Drink: Water or unsweetened beverages.
Portion Control
Portion control is essential for preventing blood sugar spikes and managing weight. Even healthy foods can lead to high blood sugar if consumed in large amounts.
1. Understanding Serving Sizes:
Learning the difference between portion size (what you serve yourself) and serving size (recommended amount) is crucial.
- Use measuring cups, spoons, or a food scale to understand standard serving sizes.
- Read nutrition labels to check serving sizes for packaged foods.
2. Mindful Eating:
Paying attention to hunger and fullness cues helps prevent overeating.
- Tips: Eat slowly, avoid distractions during meals, and savor each bite.
- Strategy: Use smaller plates and bowls to naturally reduce portion sizes.
3. Visual Portion Guides:
Simple visual cues can help with portion control:
- Protein: Palm of your hand (chicken, fish).
- Carbohydrates: A cupped hand (rice, pasta).
- Fats: Size of your thumb (butter, oils).
- Vegetables: Two cupped hands (non-starchy veggies).
4. Meal Timing and Frequency:
Eating regular, balanced meals throughout the day helps maintain steady blood sugar levels.
- Strategy: Eat smaller, balanced meals every 3–4 hours instead of large, heavy meals.
- Avoid: Skipping meals, which can lead to overeating and blood sugar fluctuations.
Importance of Regular Exercise
Exercise is one of the most effective ways to prevent and manage Type 2 diabetes. Staying active can help maintain a healthy weight, improve insulin sensitivity, and lower blood sugar levels. In addition to its physical benefits, regular exercise also has a profound impact on overall well-being, reducing the risk of other chronic diseases and enhancing quality of life.
How Staying Active Helps Reduce the Risk of Type 2 Diabetes
Regular physical activity plays a critical role in reducing the risk of developing Type 2 diabetes. Here’s how exercise contributes to better blood sugar management and overall health:
1. Improves Insulin Sensitivity
One of the primary ways exercise helps manage and prevent Type 2 diabetes is by improving insulin sensitivity.
- Insulin sensitivity refers to how effectively the body’s cells respond to insulin, the hormone that helps move glucose (sugar) from the bloodstream into cells for energy.
- Regular physical activity makes muscle cells more responsive to insulin, allowing the body to use glucose more efficiently and reducing the risk of insulin resistance, which is the primary precursor to Type 2 diabetes.
2. Helps Control Blood Sugar Levels
Exercise has an immediate and long-term effect on blood sugar levels:
- Immediate benefits: During exercise, the muscles use glucose for energy, which lowers blood sugar levels. This effect can last for hours or even up to 24 hours after physical activity.
- Long-term benefits: Consistent exercise helps maintain better overall blood sugar control, reducing the frequency and severity of blood sugar spikes.
- Risk reduction: Regular exercise decreases the chances of experiencing high blood sugar (hyperglycemia) and also lowers the risk of low blood sugar (hypoglycemia) by enhancing the body’s ability to regulate glucose.
3. Aids in Weight Management
Excess weight, particularly abdominal fat, is a significant risk factor for Type 2 diabetes. Regular physical activity is crucial for:
- Burning calories and helping with weight loss.
- Preserving muscle mass during weight loss, which is important for maintaining a healthy metabolism.
- Reducing belly fat (visceral fat), which can worsen insulin resistance.
Maintaining a healthy weight through exercise can prevent or delay the onset of Type 2 diabetes, especially for individuals who are at high risk due to family history or prediabetes.
4. Reduces Inflammation
Chronic low-grade inflammation is a key factor in the development of insulin resistance and Type 2 diabetes. Regular exercise helps to reduce systemic inflammation in the body:
- Anti-inflammatory effects: Physical activity has been shown to lower levels of inflammatory markers, improving the body’s ability to use insulin and process glucose.
- Reduced stress on the cardiovascular system: Reducing inflammation also benefits heart health, which is crucial because individuals with diabetes are at a higher risk for cardiovascular diseases.
5. Enhances Cardiovascular Health
Exercise plays a significant role in maintaining cardiovascular health, which is important for people at risk of diabetes:
- Improves heart function and lowers the risk of high blood pressure, cholesterol, and triglycerides—all risk factors for Type 2 diabetes.
- Increases blood circulation and the efficiency of the cardiovascular system, which also helps the body use glucose better.
Maintaining a healthy heart through exercise reduces the risk of complications associated with Type 2 diabetes, such as heart disease and stroke.
6. Supports Mental Health and Stress Management
Mental health plays a significant role in overall diabetes risk:
- Exercise reduces stress: Physical activity stimulates the release of endorphins (feel-good hormones), which help reduce stress and anxiety, both of which can contribute to unhealthy eating and poor lifestyle choices.
- Improves mood and motivation: Regular exercise boosts mood and can increase motivation to stick with healthy habits, like proper nutrition and medication adherence.
Stress management and mental well-being are essential for preventing Type 2 diabetes, as stress can elevate cortisol levels, which negatively affect blood sugar control.
7. Increases Energy and Stamina
Regular physical activity improves overall stamina, making it easier to perform everyday activities. More energy means:
- A more active lifestyle: The individual is more likely to engage in daily physical activity, reducing sedentary behavior that contributes to weight gain and insulin resistance.
- Sustained energy levels: With better glucose metabolism, the body has more stable energy levels, which can help with making healthier food choices and staying active.
Managing Stress and Mental Health
Stress has a profound impact on both physical and mental health, and it can significantly affect blood sugar levels in individuals with diabetes. Managing stress effectively is crucial for maintaining blood sugar control, as well as for promoting overall well-being. By recognizing the link between stress and blood sugar, individuals can take proactive steps to reduce its effects and improve their quality of life.
The Impact of Stress on Blood Sugar
Stress triggers a cascade of hormonal and physiological responses that can influence blood sugar levels. When the body perceives stress, it activates the “fight or flight” response, which prepares the body to deal with perceived threats. This response involves the release of stress hormones like adrenaline and cortisol, which can impact blood sugar in several ways:
1. Increased Blood Sugar Levels (Hyperglycemia)
- Stress hormones raise glucose levels: When stress hormones are released, the body’s liver produces more glucose (sugar) to supply energy for the “fight or flight” response. This can cause temporary spikes in blood sugar levels.
- Insulin resistance: Chronic stress can lead to increased insulin resistance, meaning that insulin becomes less effective in helping cells absorb glucose from the bloodstream, further contributing to high blood sugar.
2. Impact on Appetite and Eating Habits
- Emotional eating: Stress can lead to overeating or consuming unhealthy foods high in sugar and fat. These foods can cause blood sugar spikes and make it harder to manage diabetes.
- Hormonal changes: Stress hormones may also affect hunger-regulating hormones, leading to cravings for high-carb, sugary foods that can worsen blood sugar control.
3. Disruption of Sleep Patterns
- Poor sleep from stress: Chronic stress can interfere with sleep quality, and poor sleep is a known contributor to insulin resistance and blood sugar imbalances.
- Sleep deprivation: Lack of rest can lead to higher levels of cortisol and increased blood sugar levels the next day.
Strategies to Manage Stress
Effectively managing stress is key to maintaining stable blood sugar levels and promoting overall health. Here are some practical strategies that can help individuals reduce stress and mitigate its impact on blood sugar:
1. Mindfulness and Relaxation Techniques
- Deep breathing exercises: Slow, deep breaths can activate the parasympathetic nervous system (the body’s “rest and digest” system), counteracting the stress response. Techniques like diaphragmatic breathing or box breathing can help lower cortisol levels.
- Progressive muscle relaxation (PMR): This technique involves tensing and relaxing muscle groups to reduce physical tension and lower stress levels.
- Mindfulness meditation: Practicing mindfulness or guided meditation can help individuals stay present and calm their minds, reducing feelings of anxiety and stress.
- Yoga and Tai Chi: These mind-body exercises combine movement, breathing, and meditation to reduce stress, improve flexibility, and promote relaxation.
2. Physical Activity and Exercise
Exercise is a powerful tool for reducing stress and stabilizing blood sugar levels:
- Endorphin release: Physical activity boosts the production of endorphins, the body’s natural mood elevators, which help counteract the stress response.
- Improved sleep quality: Regular exercise helps regulate sleep patterns and can reduce the negative effects of stress on sleep.
- Reduced cortisol levels: Exercise lowers cortisol levels and helps the body process stress more effectively.
Recommended activities include walking, jogging, cycling, swimming, and activities like yoga or dancing that promote both physical and mental well-being.
3. Time Management and Setting Boundaries
Stress is often caused by feeling overwhelmed by responsibilities or the pressure to perform. Learning to manage time effectively and set boundaries can reduce stress levels:
- Prioritize tasks: Break down large tasks into smaller, manageable steps and focus on one thing at a time.
- Set realistic expectations: Recognize limitations and set achievable goals to avoid unnecessary pressure.
- Take breaks: Regular breaks throughout the day, especially during high-pressure times, can help clear the mind and reduce stress.
4. Social Support and Connection
Building a strong support network is vital for emotional well-being and stress reduction:
- Talk to loved ones: Sharing feelings with friends, family, or a therapist can provide emotional relief and help you feel more understood.
- Join support groups: Online or in-person support groups for people with diabetes can offer a sense of community and allow individuals to share coping strategies for managing stress and diabetes.
5. Adequate Sleep and Rest
Getting enough sleep is crucial for managing stress and blood sugar levels:
- Practice good sleep hygiene: Create a relaxing bedtime routine, limit screen time before bed, and maintain a consistent sleep schedule.
- Limit caffeine and alcohol intake late in the day, as these can interfere with sleep quality.
- Mind your stress levels before bed: Try relaxation techniques like reading, deep breathing, or taking a warm bath to wind down.
6. Healthy Eating and Nutritional Support
Eating well-balanced meals and managing emotional eating are essential strategies for stress management:
- Focus on balanced meals: Include whole grains, lean proteins, fruits, and vegetables to stabilize blood sugar levels and reduce cravings.
- Avoid stress-induced overeating: When stressed, it’s easy to reach for unhealthy comfort foods, which can spike blood sugar. Aim to eat regular, nutritious meals to avoid emotional eating.
7. Professional Support: Therapy and Counseling
For those experiencing chronic stress, anxiety, or depression, professional help may be beneficial:
- Cognitive Behavioral Therapy (CBT): This therapy focuses on identifying and changing negative thought patterns that contribute to stress and anxiety.
- Stress management programs: Therapy or counseling can help develop coping mechanisms for managing stress in a healthier way.
Routine Health Check-ups
Routine health check-ups are essential for anyone with diabetes or at risk of developing diabetes. These regular appointments with healthcare professionals allow for early detection, timely intervention, and effective management of the condition. Regular monitoring of blood sugar levels and consistent visits to a healthcare provider can help prevent complications, keep blood sugar within the target range, and improve the overall quality of life.
Regular Blood Sugar Monitoring
Monitoring blood sugar levels is the cornerstone of managing diabetes. Regular blood sugar checks help individuals understand how well they are managing their diabetes and whether their current treatment plan is effective. It also helps to identify trends or patterns that could indicate the need for adjustments in diet, exercise, or medication.
1. Importance of Self-Monitoring
Self-monitoring of blood glucose (SMBG) is a vital tool for daily diabetes management:
- Tracking blood sugar: Regular checks allow individuals to track their blood sugar levels throughout the day. It’s especially important to monitor levels before and after meals, as well as before physical activity.
- Immediate feedback: By testing blood sugar, individuals get immediate feedback about the effectiveness of their lifestyle choices (e.g., food intake, exercise, medication adherence). This can help make adjustments in real time.
- Identifying high or low levels: Regular blood sugar checks can help identify periods of hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar), allowing individuals to take prompt action to address the situation.
2. A1C Testing for Long-Term Blood Sugar Control
In addition to daily blood glucose monitoring, individuals with diabetes should have an A1C test performed regularly (usually every three months). This test provides a broader picture of how well blood sugar has been controlled over a period of time, as it measures the average blood glucose levels over the past two to three months.
- Target A1C levels: The American Diabetes Association recommends an A1C level of less than 7% for most adults with diabetes. A higher A1C level can indicate that blood sugar levels have been elevated over an extended period, increasing the risk of complications.
3. Continuous Glucose Monitoring (CGM)
For individuals with Type 1 diabetes or those struggling to manage blood sugar levels with traditional methods, continuous glucose monitoring (CGM) can provide real-time data on blood sugar trends. A small sensor placed under the skin measures blood sugar throughout the day and night, offering more frequent updates and insights into fluctuations. This technology helps reduce the risk of both high and low blood sugar events.
Doctor Visits for Early Prevention
Regular doctor visits are vital for individuals with diabetes or those at risk for the condition. These appointments allow healthcare professionals to monitor overall health, adjust treatments, and screen for potential complications. Early detection and intervention are key in preventing long-term health problems and managing diabetes effectively.
1. Comprehensive Diabetes Management
At routine doctor visits, a healthcare provider will assess how well an individual is managing their diabetes:
- Review of blood sugar levels: The doctor will discuss recent blood glucose readings and A1C test results to determine if adjustments are needed in the treatment plan.
- Medication adjustments: Based on blood sugar trends, the doctor may recommend adjustments to insulin therapy or oral medications to improve blood sugar control.
- Nutrition and exercise advice: The doctor may offer guidance on diet, exercise, and lifestyle changes to help manage blood sugar and prevent complications.
2. Screening for Complications
Early detection of complications is critical for individuals with diabetes. Routine check-ups provide an opportunity for healthcare professionals to screen for potential diabetes-related issues:
- Eye exams: Diabetic retinopathy is a common complication of diabetes that can lead to blindness if untreated. Regular eye exams by an ophthalmologist can help detect signs of damage to the blood vessels in the eyes before vision loss occurs.
- Kidney function tests: Kidney damage (diabetic nephropathy) is another common complication of diabetes. Regular urine tests and blood pressure checks can help detect early signs of kidney damage, allowing for early intervention.
- Nerve function tests: Diabetes can damage nerves, leading to diabetic neuropathy. Routine check-ups often include tests to assess nerve function, especially in the feet and legs, to prevent complications like infections or amputations.
- Blood pressure and cholesterol checks: Diabetes increases the risk of cardiovascular disease, so regular monitoring of blood pressure and cholesterol levels is essential for preventing heart disease and stroke.
3. Monitoring Mental Health
Managing a chronic condition like diabetes can take a toll on mental health. Regular visits to the doctor also provide an opportunity to assess mental health and address issues like stress, anxiety, or depression, which can affect diabetes management:
- Mental health screenings: The doctor may ask about emotional well-being, offer referrals to therapists or counselors, or recommend stress-management techniques to improve overall quality of life.
- Supportive counseling: Emotional support and encouragement from the healthcare provider can help individuals cope with the psychological challenges of living with diabetes.
4. Vaccinations and Preventive Care
Individuals with diabetes are at a higher risk of infections and illnesses, so routine health check-ups should also include updates on recommended vaccinations:
- Flu and pneumonia vaccines: People with diabetes are more susceptible to infections, so vaccinations like the flu shot and pneumonia vaccine can help protect against respiratory illnesses.
- Hepatitis B vaccination: Diabetic patients, especially those who are insulin-dependent, may be at a higher risk for hepatitis B, so vaccination is often recommended.
5. Personalized Health Goals
During routine doctor visits, the healthcare provider will work with the individual to set personalized health goals based on their unique needs, lifestyle, and diabetes management:
- Target blood sugar levels and A1C goals.
- Exercise and diet plans tailored to the individual’s preferences and capabilities.
- Medication strategies that align with personal schedules and health priorities.
Conclusion:
Understanding the basics of diabetes is the first step toward effective management and prevention. Diabetes is a complex condition that impacts various aspects of health, from blood sugar regulation to the potential development of serious complications. By familiarizing yourself with the key concepts—such as the types of diabetes, how insulin works, common symptoms, and the importance of regular monitoring—you empower yourself to make informed decisions about your health. This knowledge forms the foundation for better prevention, early detection, and successful management of the disease.
Taking control of your health is essential. Regular check-ups, blood sugar monitoring, and lifestyle adjustments can make a significant difference in managing diabetes and preventing complications. It’s not just about understanding the condition, but also actively working with your healthcare team to tailor a treatment plan that fits your individual needs. Your doctor, nutritionist, and other healthcare professionals are valuable resources in navigating the challenges of diabetes, and their expertise can guide you toward a healthier future.
Remember, diabetes management is a continuous journey. It requires attention, commitment, and regular monitoring to stay on top of your blood sugar levels. Be proactive—check your blood sugar regularly and seek professional guidance if you notice any symptoms or changes in your health. Early intervention and careful management can significantly reduce the risk of long-term complications like nerve damage, kidney issues, and cardiovascular problems.
Call to Action:
- Take charge of your health today—schedule a check-up, monitor your blood sugar regularly, and stay informed about the best practices for managing diabetes.
- Stay in tune with your body: If you experience any changes in your symptoms, don’t hesitate to consult with your healthcare provider for guidance.
- Commit to regular monitoring: Regular blood sugar checks and routine doctor visits are essential for early detection and prevention of complications.
By staying informed, taking small but consistent steps, and seeking the right medical support, you can manage diabetes effectively and live a fulfilling life. Your health is in your hands—take the first step toward a healthier future today.
FAQ – Frequently Asked Questions About Diabetes
What is the difference between Type 1 and Type 2 Diabetes?
Type 1 diabetes is an autoimmune disease where the immune system attacks the insulin-producing cells in the pancreas.
Type 2 diabetes occurs when the body becomes resistant to insulin or doesn’t produce enough insulin.
What are the early signs of diabetes?
Common symptoms include excessive thirst, frequent urination, extreme fatigue, blurred vision, and unexplained weight loss.
Can diabetes be cured?
Currently, there is no cure for diabetes, but it can be managed effectively with a balanced diet, exercise, and medication.
Can Type 2 diabetes be prevented?
Yes, by adopting a healthy lifestyle, maintaining a healthy weight, eating a balanced diet, and exercising regularly, you can significantly reduce the risk of developing Type 2 diabetes.
What treatments are available for diabetes?
Treatment includes managing blood sugar levels with medications (such as insulin and metformin), a proper diet, and regular physical activity. Patients may also use blood glucose monitoring devices.
Can diabetes lead to serious complications?
Yes, if left untreated or poorly managed, diabetes can lead to serious complications such as heart disease, nerve damage (neuropathy), kidney problems (nephropathy), and vision problems (retinopathy).
How can I know if I’m at risk for diabetes?
If you have a family history of diabetes, a sedentary lifestyle, a diet high in sugars or fats, or are overweight, you may be at risk. It’s essential to consult with a doctor for early diagnosis.
Main References: DIABETES
















