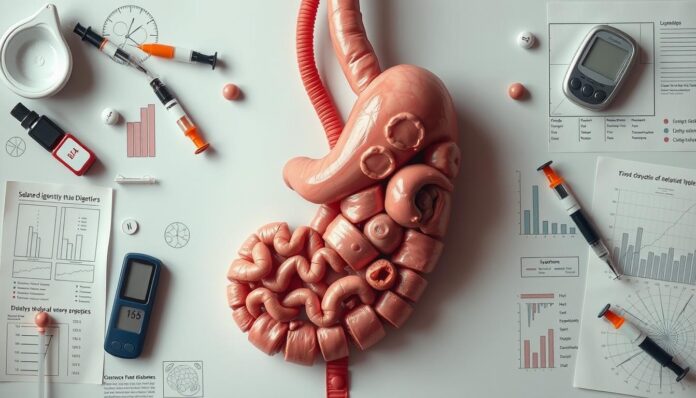
Living with diabetes can be tough, and diabetes gastroparesis makes it even harder. You might feel nauseous, vomit, or get full quickly, even after eating a little. It’s important to know about diabetes gastroparesis, its symptoms, and treatment options to manage it well.
Understanding diabetes gastroparesis is key. Knowing its causes, symptoms, and treatments helps you take charge of your health. Whether your symptoms are mild or severe, the right action can greatly improve your life.
Key Takeaways
- Diabetes gastroparesis is a complication of diabetes that affects the stomach’s ability to empty its contents into the small intestine.
- Recognizing diabetic gastroparesis symptoms, such as nausea and vomiting, is crucial for early diagnosis and treatment.
- Gastroparesis treatment options are available to help manage symptoms and improve quality of life.
- Understanding the causes of diabetes gastroparesis can help you make informed decisions about your care.
- Staying informed about diabetes gastroparesis can empower you to take control of your condition and improve your overall well-being.
- Exploring available gastroparesis treatment options can help you find the best course of action for your specific needs.
Understanding Diabetes Gastroparesis
When you learn about diabetes, you might hear about gastroparesis definition. It’s when your stomach takes too long to empty food. This often happens in people with diabetes. High blood sugar can damage nerves that control the stomach, causing gastroparesis.
This damage slows down how food moves into the small intestine. It’s important to manage your diabetes well to avoid gastroparesis. Keeping your blood sugar levels in check can prevent nerve damage and gastroparesis.
Working with your healthcare provider is key. They can help you create a plan to manage your diabetes and prevent gastroparesis.
Some important things to think about in diabetes management and preventing gastroparesis include:
- Eating smaller, more frequent meals to reduce the burden on the stomach
- Choosing foods that are low in fat and fiber, which can be easier to digest
- Avoiding foods that can trigger symptoms, such as carbonated beverages or spicy foods
Understanding the link between diabetes and gastroparesis helps you manage your condition better. Always work with your healthcare provider to create a plan for diabetes management and preventing gastroparesis.
Common Signs and Symptoms You Should Know
It’s important to know the symptoms of gastroparesis to get medical help quickly. You might feel nauseous, vomit, have bloating, or feel full too soon after eating. These signs can be similar to other health issues, so getting a correct diagnosis is key. If you live with gastroparesis, being aware of these symptoms and knowing when to ask for help is crucial.
Some key symptoms to look out for include:
- Nausea and vomiting
- Bloating and abdominal discomfort
- Feeling full after eating very little
- Weight loss and malnutrition
Diabetic gastroparesis symptoms can be like those of other conditions. So, it’s important to see a doctor for a proper diagnosis. Knowing the symptoms of gastroparesis is the first step to managing it and improving your life. To live well with gastroparesis, you need to make dietary changes, take medication, and adjust your lifestyle.
By recognizing gastroparesis symptoms and getting medical help, you can start managing your condition. This will help you live more comfortably, even with the challenges of gastroparesis. Early recognition and treatment are key to avoiding complications and improving your health.
Diagnosis Process and Tests
If you’re showing signs of gastroparesis, getting a proper diagnosis is key. The gastroparesis diagnosis involves looking at your medical history and doing a physical check-up. A crucial test is the gastric emptying study, which checks how fast food leaves your stomach.
Other tests might include:
- Upper endoscopy to see the upper digestive tract
- Imaging tests, like X-rays or ultrasound, to check for other causes
- Blood work to find diabetes complications or other issues
Knowing about the diagnostic process can prepare you. It’s important to work with your doctor to find the right steps for you. Tests for gastroparesis help find the cause of your symptoms, which is vital for treatment.
These tests help you understand your condition better. Remember, diabetes complications can raise your risk of gastroparesis. So, it’s crucial to keep an eye on your health and work with your doctor to avoid more problems.
Managing Your Diet with Diabetes Gastroparesis
To manage your gastroparesis diet, making specific changes is key. Eating smaller, more frequent meals can ease digestion. Choosing low-fat and low-fiber foods also helps. A healthcare provider or dietitian can give you personalized advice, including diabetes meal planning.
Some general dietary recommendations for gastroparesis diet include:
- Eating smaller, more frequent meals throughout the day
- Choosing low-fat and low-fiber foods, such as lean proteins, low-fiber fruits, and vegetables
- Avoiding carbonated beverages and alcohol, which can exacerbate symptoms
By following these tips, you can reduce discomfort and manage symptoms. It’s crucial to work with a healthcare provider. They can help you create a diabetes meal plan that fits your needs and health goals.
Also, keeping a food diary can track which foods trigger symptoms. This info helps in creating a personalized diet plan. With the right dietary choices and healthcare support, you can better manage your symptoms and improve your health.
Medical Treatment Options Available
Managing gastroparesis has several treatment options. Your doctor might give you medications for gastroparesis. These help the stomach muscles contract, which aids in food digestion.
Some key treatment options include:
- Medications to stimulate stomach muscle contractions
- Medications to control nausea and vomiting
- Diabetes treatment to manage blood sugar levels
It’s crucial to work with your healthcare provider to create a treatment plan that fits your needs. In severe cases, treatments like jejunostomy tubes might be considered.
Understanding the gastroparesis treatment options and following your doctor’s advice can help manage symptoms. Always take your medications for gastroparesis as directed for the best results.
Conclusion: Living Well with Gastroparesis
Living well with gastroparesis means being proactive. Work closely with your healthcare team to manage your condition. This can greatly improve your life quality.
Changing your lifestyle is key. Follow a diet that works for you and stay active. This can help a lot with your symptoms. Also, getting support from loved ones or support groups can offer emotional and practical help.
You’re not alone in this fight. Many people with diabetes gastroparesis have found ways to thrive. With determination and a positive attitude, you can manage your condition well.
Stay informed and speak up for what you need. Don’t be afraid to ask for help when you need it. By doing these things, you can enjoy life fully, even with gastroparesis.
FAQ
What is diabetes gastroparesis?
Diabetes gastroparesis is a problem that happens when you have diabetes. It makes it hard for your stomach to empty food into your small intestine. This can cause nausea, vomiting, and feeling full quickly, even after eating a little.
What causes diabetes gastroparesis?
Long-term high blood sugar can damage the nerves that control your stomach. This damage slows down how food moves from your stomach to your small intestine.
What are the common symptoms of gastroparesis?
Symptoms include nausea, vomiting, bloating, and feeling full too soon. These can be similar to other conditions, so getting a correct diagnosis is key.
How is diabetes gastroparesis diagnosed?
Doctors use your medical history, a physical exam, and tests like a gastric emptying study. They might also do an upper endoscopy and imaging tests.
How can I manage my diet with diabetes gastroparesis?
Eat small meals often and choose foods low in fat and fiber. Avoid carbonated drinks. A healthcare provider or dietitian can help create a diet plan for you.
What medical treatment options are available for gastroparesis?
Treatments include medicines to help your stomach move and control nausea and vomiting. They also help manage your blood sugar. In some cases, a jejunostomy tube might be needed.
How can I live well with gastroparesis?
To live well, work closely with your healthcare team and make lifestyle changes. Seek support from loved ones or support groups. By managing your condition and staying informed, you can enjoy life despite gastroparesis.
Main References: National Library of Medicine